Disclaimer:
This article is for information purposes only. It is not a substitute for medical advice or treatment. Seek medical care for your treatment.
What is Hemolytic anemia?
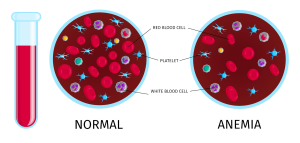
Hemolytic anemia is a type of anemia. Anemia refers to a condition in which the blood has a lower than normal number of red blood cells. Hemolytic anemia is a sub-type of anemia, a general disorder that develops when the body has lesser red bood cells than normal. The low red blood cell count in hemolytic anemia results from the deterioration of red blood cells rather than from their underproduction. When red blood cells perish more quickly than the bone marrow can produce them, it happens. All bodily parts receive oxygen from the lungs via red blood cells.
Causes of hemolytic anemia:
There are several causes of hemolytic anemia that can be divided into several categories. Hemolytic anemia can be due to acquired or inherited causes. The term “acquired hemolytic anemia” indicates the beginning of illness in individuals whose red blood cells had previously been functioning normally. Conversely, some people may inherit this illness from their parents and have it from birth.
Types of hemolytic anemia:
There are various types of hemolytic anemia. The condition can be:
- Inherited: This means that the parents have passed on the gene for the condition to you.
- Acquired: means that you are not born with this condition but you may develop it over time.
- Inherited hemolytic anemia:
One or more of the genes that govern the generation of red blood cells have failed in hereditary hemolytic anemia. This may result in issues with the enzymes that keep healthy red blood cells intact, hemoglobin, or the cell membrane.
It’s possible that the abnormal cells are fragile and degrade as they pass through the circulation. The spleen, an organ, could remove the cell debris from the bloodstream in this scenario.
- Sickle cell anemia:
Sickle cell anemia is a chronic, inherited disease. In this condition body makes aberrant hemoglobin. This leads the red blood cells to have a sickle or crescent shape. Sickle cells have a shorter lifespan than healthy red blood cells. They perish after 10-20 days. Red blood cells can’t be produced quickly by bone marrow to substitute the dying ones. In the United States, African Americans are mostly affected by sickle cell anemia.
- Hereditary Spherocytosis:
Red blood cells in this disease have a deficiency in their external membrane, or outer covering, which gives them a spherical or ball-like shape. The lifespan of these blood cells is shortened compared to normal.
For individuals of Northern European heritage, the most frequent cause of hemolytic anemia is hereditary spherocytosis.
- Hereditary Elliptocytosis:
In this condition the red blood cells are elliptic in shape. They are not as pliable as normal red blood cells and have a shorter lifespan.
- G6PD deficiency:
In G6PD deficiency, the red blood cells lack a significant enzyme called G6PD. In G6PD deficiency, if red blood cells come in contact with some substances in the bloodstream, the absent enzyme causes the cells to burst and expire. Many elements can activate the breakdown of the red blood cells. G6PD deficiency mostly affects males of African or Mediterranean descent. In the United States the condition is more frequent among African Americans than Caucasians.
- Thalassemia:
Thalassemia is an inherited blood condition in which body fails to produce sufficient hemoglobin. This makes the body to produce lesser healthy red blood cells than normal. Generally people of Southeast Asian, Indian, Chinese, Filipino, Mediterranean or African origin are affected by thalassemia.
- Pyruvate Kinase Deficiency:
In this body is lacking an enzyme called pyruvate kinase. Lack of this enzyme causes red blood cells to collapse easily. This disorder is more frequent among the Amish than other groups.
- Acquired Hemolytic Anemia:
Your red blood cells may be normal with the acquired hemolytic anemia. However, some other disease or factor makes the body to damage the red blood cells and eradicate them from the bloodstream. The demolition of the red blood cells happens in the blood stream or more frequently in the spleen.
- Immune Hemolytic Anemia:
In immune hemolytic anemia the red blood cells are damaged by your immune system. The three main types of immune hemolytic anemia are autoimmune, all immune and drug induced.
- Autoimmune hemolytic anemia: in this condition, your immune system makes antibodies that strike your red blood cells. Why AIHA happens is not known. Half of all cases of hemolytic anemia are caused by AIHA. AIHA has the potential to develop rapidly and seriously. Having some diseases or infections can increase your risk for AIHA. Examples are:
- Autoimmune diseases
- Chronic lymphocytic leukemia
- Non-Hodgkin’s lymphoma and other blood cancers
- Epstein-Barr virus
- Cytomegalovirus
- Mycoplasma pneumonia
- Hepatitis
- HIV
AIHA can occur after a blood and marrow stem cell transplant. In some types of AIH, the antibodies made by the body are called antibodies. In other types of AHIA, the body makes cold-reactive antibodies.
- All immune hemolytic anemia: this type of hemolytic anemia develops if your body makes antibodies against red blood cells that you get from a blood transfusion. This happens when the transfused blood is a different blood type than your blood. This type of hemolytic anemia can develop during pregnancy if a woman has Rh-negative blood and her baby has Rh-positive blood.
- Drug-induced hemolytic anemia:
Some medicines can develop a reaction that causes hemolytic anemia. Some medicines such as penicillin, bind to red blood cell surfaces and cause antibodies to develop. Certain medicines cause hemolytic anemia in other ways.
- Mechanical hemolytic anemia:
Physical harm to red blood cells membranes can cause their break down faster than normal. Damage may be due to:
- An artificial heart valve or other device used in blood vessels
- Hemodialysis
- Heart-lung bypass machine
- Changes in the small blood vessels
- Preeclampsia or eclampsia
- Malignant hypertension
- Thrombotic thrombocytopenic purpura
- Strenuous activities can also lead to blood cell damage
- Paroxysmal Nocturnal Hemoglobinuria:
PNH is a condition in which red blood cells are defective due to shortage of certain proteins. The body harms these cells more abruptly than normal. People with PNH are at great risk for blood clots in the veins and decreased levels of white blood cells and platelets.
Certain substances and infections can also cause damage to red blood cells and lead to hemolytic anemia.
Conclusion:
There are various types of hemolytic anemia. Your treatment and outlook is based on the severity and the type you have. The condition can happen gradually or suddenly and symptoms can vary from mild to chronic. Generally hemolytic anemia can be controlled and treated successfully. Mild hemolytic anemia requires no treatment whereas, severe hemolytic anemia needs immediate treatment.